New Hips for Next Summer

In 2014, I walked more miles than I’ve ever walked in a year. Megan and I had been taking frequent long walks and hikes with the dogs in recent years, but we really kicked it up a notch when we started preparing for a trekking vacation in Dartmoor National Park last year.

We walked many places around the Seattle area, including the 18 miles from our home to work (twice) as well as the 20 miles around Lake Sammamish in a day, and the 7 miles around Lake Union in an evening. To circumambulate Lake Washington we set aside three days, but after a 28-mile second day from Redmond around the north end of the lake and down to the U District, we skipped the last 11 miles. We spent a Saturday walking the 19 miles of the Green River Trail through Kent and Tukwila, and we took countless shorter walks around Seward Park, Green Lake and other Seattle neighborhoods.

We took hikes in the mountains, too, ranging from short steep trails like Sauk Mountain or High Rock Lookout to longer day hikes like Earl Peak. We did Beckler Peak, Skyline Divide, and our favorite trails all up and down the Middle Fork Snoqualmie River valley, many times each.
I usually took Ibuprofen before and after hikes, and often found it difficult to sleep after a long day. My hip joints ached, and sometimes my muscles felt even more pain than the joints. But the particular muscle involved would change suddenly from the inside to the outside edge of the thigh, and at times the muscles hurt while sitting still but felt much better when I worked them hard. In hindsight, I spent months trying to pinpoint a specific problem when the answer was more general: everything around my hip joints was starting to hurt.
In May of 2014, I had my annual checkup and complained to my doctor of the pain in my left hip. She said we should get it x-rayed to be sure there wasn’t a fracture, and the radiologist’s report concluded “osteoarthritis, with mild joint space narrowing, circumferential femoral head marginal spurring, and no evidence of left hip fracture.”
At the time, that seemed a good outcome — the pain wasn’t due to something bad like a fracture, it was just plain old arthritis! Most people get arthritis eventually, and my turn was coming.
The problem seemed easily manageable. On the way through London headed for Dartmoor, we stocked up on Nurofen Plus (Ibuprofen with codeine, available over the counter in the UK but not the US). For the rest of our vacation, my first task after long days on the trails was to get to the nearest pub and wash down a couple of Nurofen Plus tabs with a cider.
We had a great time on our Dartmoor trekking vacation, but my arthritic hips were wearing out with every step.




Then things went further downhill after we returned. I knew I had arthritis, but I didn’t realize how quickly the cartilage was grinding away. The fact I could no longer put either foot on the opposite knee while sitting was obvious, but more subtle were the recurring problems (cramping, spasms, aches and pains) in my quads and other leg muscles. It now seems likely that these issues were caused by changes in geometry that were brought on by the deterioration of my hip joints, but at the time I kept thinking I just needed to get in better shape, or stretch more.
My hips often ached at night, and sometimes even Nurofen Plus couldn’t give me a decent night’s sleep. I found myself making excuses to not go on planned hikes, and planning fewer hikes in general.

Learning the Truth
At my annual checkup in May of this year, I talked to my doctor about these changes, and she recommended that I meet with Dr. James Bruckner, an orthopedic surgeon in the Seattle area who specializes in hip and knee reconstructions and replacements. It took me over two months to get in to see Dr. Bruckner, but I took that as a good sign: he’s clearly in demand.
My appointment finally came on July 29, and after an examination and x-rays his diagnosis was a mouthful of big words: “End-stage osteoarthritis of both hips secondary to femoral acetabular impingement, manifested by the classic anterosuperior cartilage loss. Articular cyst formation in the acetabulum, circumferential femoral head osteophytes, and acetabular osteophytes.”
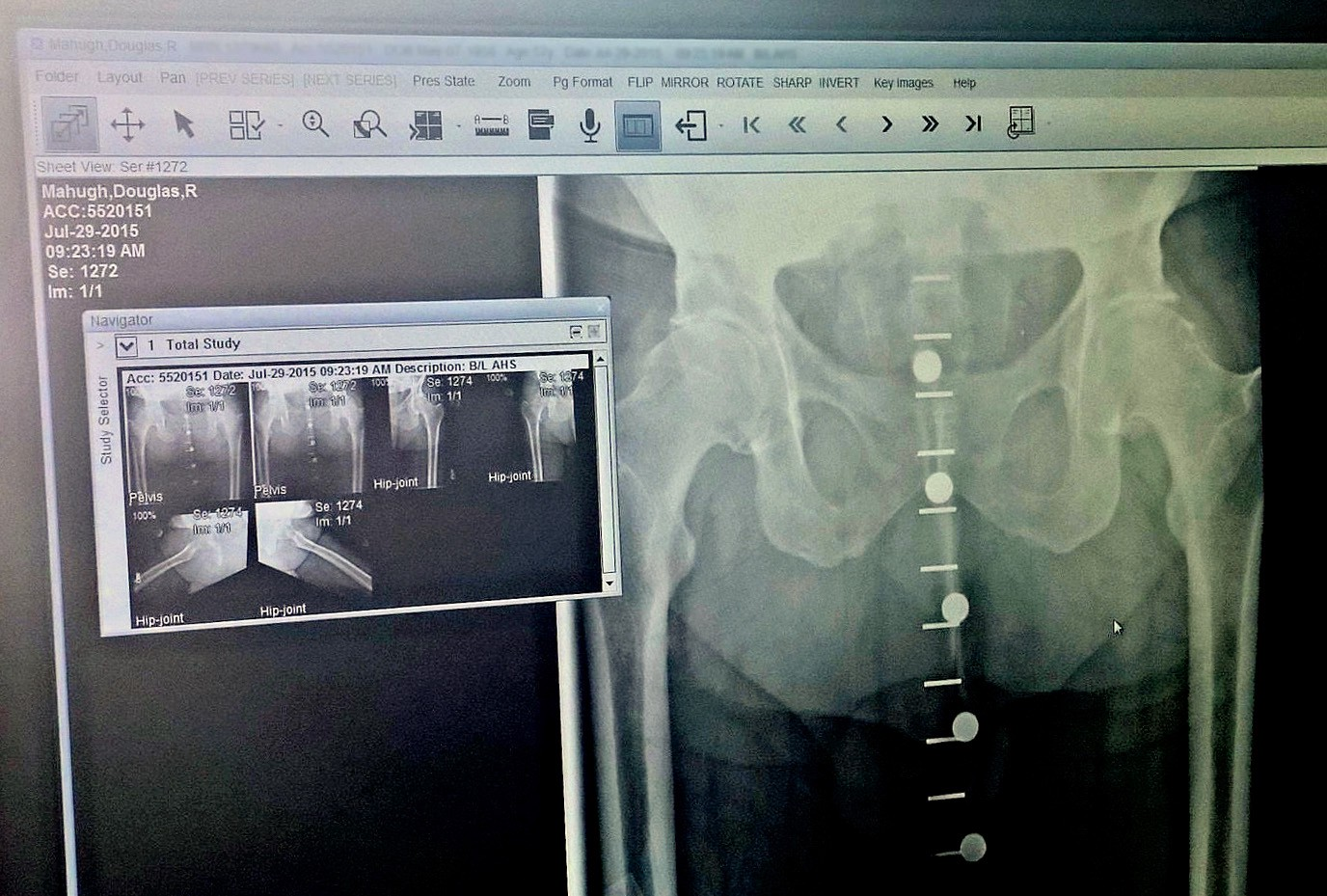
End-stage didn’t sound good, and Dr. Bruckner showed me how the x-rays compared with those taken one year before. Most of the remaining cartilage in both hip joints had worn away in just one year. Another active year and my hips would be bone on bone, but that wasn’t likely to happen, because hip pain was preventing me from having an active year.
I mulled it over and discussed with Megan, but the answer seemed pretty obvious: to do the things I enjoy doing and to stay active and healthy, I needed new hip joints. Both of them. I could put it off for a while, but it was already affecting my quality of life, and I’d never again be as strong for the recovery process as I am this year, especially if I started slowing down and getting less exercise.
One thing that seems to give some people pause on making a joint-replacement decision is the painful PT (physical therapy) process after surgery. But I went through so many months of pain while working out and preparing for Dartmoor that I felt like I’d already gone through a lot of inconvenience without actually addressing the root problem. PT couldn’t possibly be any worse than trying to be an active hiker with hips like mine, and PT doesn’t last forever!
In hindsight, it wasn’t a hard decision at all. Two days after meeting Dr. Bruckner, I made an appointment to have my right hip replaced on September 1. Full hip arthroplasty — this procedure.
Getting Ready
Once the decision was made, I started preparing for surgery. I worked with an excellent trainer, Stephanie Levine, who gave me a “pre-hab” routine to do several times a week: walking with bands around my ankles and knees, various bridges and planks to strength my glutes and core, and related exercises including sessions on a spin bike to strengthen my quads.

Meanwhile, I also worked with a nutritionist, Andrea Walker, to get my body ready for rapid recovery from surgery. She had many great suggestions, including eliminating grains from my diet to reduce inflammation and adding lots of protein and iron and zinc, to prepare for bone growth and regeneration. I even stopped drinking alcohol — we made a couple of minor exceptions for long-planned social events, but August was surely the lowest monthly alcohol intake of my adult life. Between the diet and exercise routines, I was feeling better and better as the big day approached.

Another area of preparation was our home. We moved our king-size bed from upstairs down to the guest room next to the bathroom, and got rid of a bunch of clutter to make it easy to get around after surgery. I installed a sturdy handrail next to the toilet, and bought a cane, a walker, and all the other gadgets that occupational therapists recommend for hip surgery patients.
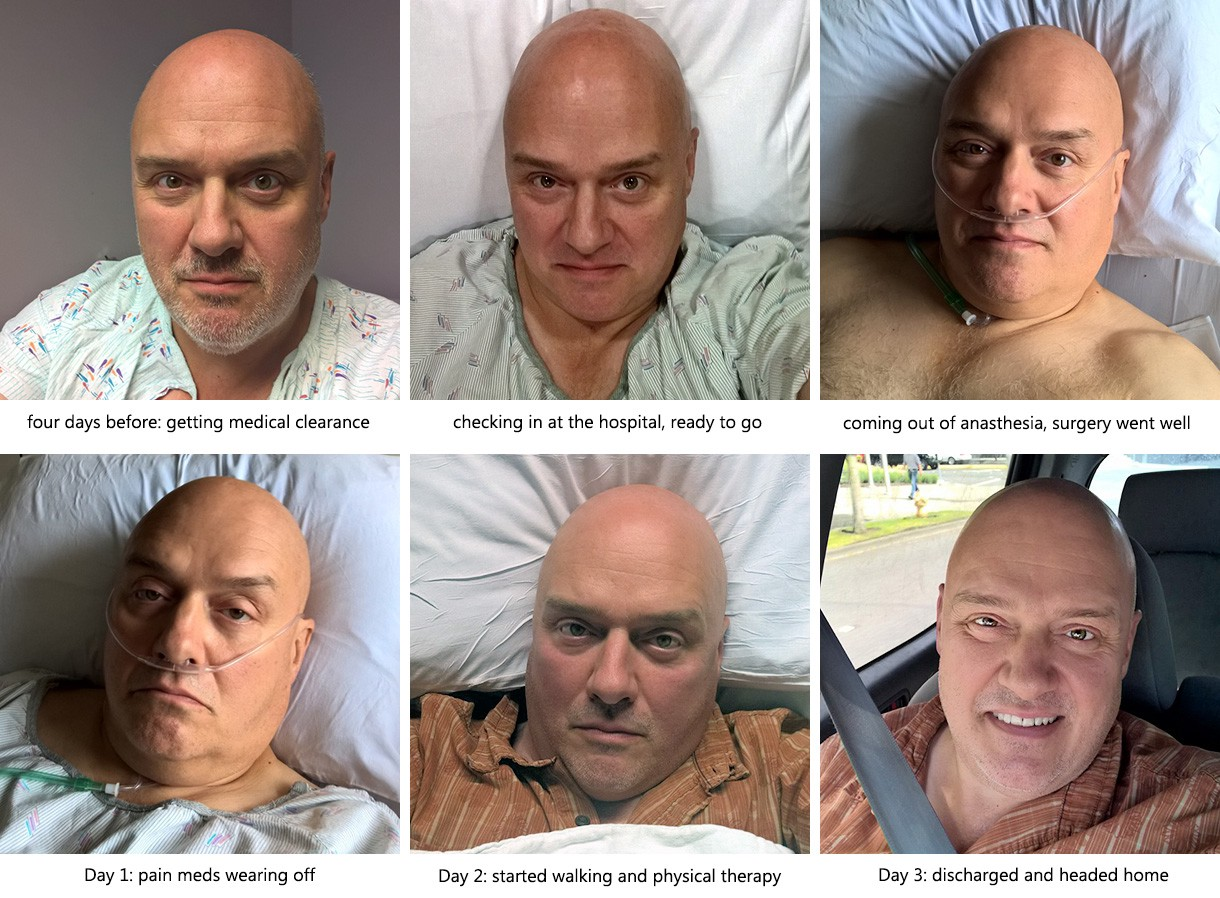
The final preparations were the various medical appointments involved: surgical clearance from my doctor, consultations with Dr. Bruckner’s PA and Overlake Hospital, and a “hip class” to learn about what to expect. I had a long day of appointments four days before surgery, and was finally ready for my first hip replacement.
The Big Day
I was scheduled for surgery at 9:50AM and checkin at 7:45, but of course we were up early and arrived at the hospital well ahead of time. The checkin process went smoothly, and I felt lucky that I liked every person involved: nurses, doctors, the PA (physician’s assistant), the anesthesiologist and all the others. Good to feel good about the folks who are about to slice me open. They had many little rituals which I found interesting: putting IVs in both arms, drawing blood, marking the spot on my feet where my pulse was strongest (so they could compare the strength of pulse in those spots after the surgery), and so on.

My favorite pre-surgery memory was the trip through the hallways of Overlake after the site-marking ritual, looking down past my raised toes while one doctor pushed my bed at a brisk pace and another walked at my side. I was hyper-alert, and soaking up every little detail. Show time!
We arrived in the operating room, and I have only a fleeting memory of the masked faces behind breathing apparatuses. (To reduce risk of infection, they were all breathing recirculated air.)
The next thing I knew, I was hearing multiple voices saying my name over and over, and I opened my eyes to the bright lights of the post-op recovery room. I felt nothing at all from around my waist to my ankles, having had both a spinal and general anesthesia.
The first order of business was to confirm that I could wiggle my toes. Check. I could feel pressure on my right toes (the side of the surgery) but not the left. This seemed backward to me, but they assured me this isn’t uncommon. All my vitals were fine, and I was quickly cleared to be discharged to my waiting hospital room.
Back in my Room
I was in the hospital room for a few minutes, and then Megan arrived. She had already met with Dr. Bruckner after the surgery, so she knew it went smoothly with no complications and everything was looking good. Which brings me to a key point: there was never a moment all day long when we were worried. We took the experience very seriously, but I would not describe this as a stressful experience. Kudos to the Proliance and Overlake teams for making it all feel that way, because we know there are real risks involved but we always felt like I was in good hands.

I had a lot of hardware hooked up to me at this point. A few things I can remember: oxygen tubes in my nostrils, an IV in my left arm (capped, but used to administer various drugs from time to time), an IV in my right arm keeping me hydrated with saline fluids, a catheter, a pulse oximeter taped to my right middle finger, and a drain device attached to my right thigh.
The drain was the most interesting of these devices, and also the noisiest and creepiest. It’s basically a tube going into the hip that steadily sucks the drainage caused by the removal of so much flesh and bone. But it doesn’t just drain the injured area, it’s also about mitigating one of the risks of hip surgery: the possible need for a blood transfusion if your blood counts drop too low.

So the drained material isn’t discarded, rather it goes to a centrifuge on a stand next to the bed, where it’s separated into blood and plasma (and possibly other stuff — I certainly don’t know the details). That way, if a transfusion were needed, I could get my own blood back, which is less risky than getting another person’s blood.
As it turned out, I didn’t need a transfusion, but this device sat next to my bed sucking and spinning and churning for 20 hours, with a big bag of blood hanging off the side of it. I was relieved when they came to remove the drain, then momentarily horrified when I saw the 5 inches of bloody tubing that had been running into the center of my thigh. One of those “I’m glad you know what you’re doing here” moments.
Constant Motion
Roughly speaking, I was in the hospital for around 48 hours. During the first 24 hours, I think I was never alone for a full hour, and during the second 24 hours I think I was left to myself for a full two hours twice. So this wasn’t about catching up on sleep, and almost every time anyone came into my room they asked me to move in some way.
The most common request was “wiggle your toes for me.” I found myself pretending the nurses and doctors were wearing t-shirts with that slogan on them, and I’d start wiggling my toes whenever I heard footsteps approaching. The specific motion they want to see is pumping your ankles, with your feet leaning toward your head and then the opposite direction, back and forth.
The other two exercises I did dozens of times, at least once an hour, were sets of ten isometric quads and glutes exercises. To activate the quads while laying down, you tighten the top of your thighs so that your heels raise slightly off the bed and hold for 5 seconds. To tighten the glutes, you just squeeze your butt together tight, to the point where there’s a slight sensation of your core raising up.

Those and deep-breathing exercises were the constants. The deep breathing is both to assure you get plenty of oxygen for healing, and also to avoid getting pneumonia while you’re laying on your back for a day or two.
Three more recurring exercises were introduced by the physical therapist when we met on Day 2: raising the knees a few inches (by sliding your heels toward your butt), lower leg raises (with a tightly wrapped towel under the knees), and sliding your feet out to the sides a few inches and then back to shoulder width.
Those were the things I was told to do, and it’s worth noting that there are also four things I was told never to do, at least until the six week follow-up appointment with the surgeon:
#1: do not bend at the waist 90 degrees or more. This is mostly an issue in getting in and out of chairs.
#2: do not rotate the new-hip foot in or out. You need to keep it straight while the joint is healing, and it’s especially important not to turn it in (i.e., pigeon-toed).
#3: do not cross the legs. Ideally, you shouldn’t even bring the feet together. That’s why you have to sleep on your back with a pillow between your legs, or on your good side with a cushion device strapped between your legs.
#4: don’t let the new hip rotate back more than 10 degrees relative to your spine. Apparently this one isn’t always stipulated (so you’ll find references to “the three hip replacement restrictions”), but it was for me.
As a final item regarding post-op exercises, here’s something that I learned from Stephanie the trainer well before surgery, but found quite helpful during my hospital stay and in the days since. Like many people who sit at a desk for a living, I have a tendency to get a sore lower back at times. And the exercise that best helps me get rid of back pain is the “sea turtle,” where you lay on your stomach and then tighten the muscles of your back enough to pull your feet and shoulders off the ground. This exercise:
In the hospital, I did “isometric sea turtles” often while laying on my back. In other words, tightening the muscles of my back enough to feel like my shoulders and feet were pressing down into the bed. My back has felt great through this whole experience, and I’m pretty sure the sea turtles have been helping.
Walking!
All this other stuff is just the details, right? The main thing everyone wants to know is “how soon can I walk?”
With the procedure I had, the answer is “right away.” They have a goal of getting you up to walk a few steps within a few hours of the surgery. In my case, my blood pressure and pulse rate were very low at that point in time, which made me dizzy when I sat up on the side of the bed. So we erred on the side of caution, and I didn’t walk then.
I finally had my first walk down to the nurse’s station and back at 3AM the first night using a walker, with a nurse holding onto a strap around my chest as a safeguard. It was about 100 feet total, and about 16 hours after the surgery. I felt some pain, but I could put my entire weight on the new hip. It was physically stable, but my brain was rebelling: “danger, danger, don’t trust this thing, what the hell is going on here?!?!” The nurse assured me that sort of self-talk is the norm at that point in the process.
I then walked a bit every few hours, and on the evening of the second day I walked a 400-foot loop around the 3rd Floor East ward where I was staying. To me, this is the most amazing aspect of the whole process, the fact that you can walk right away. It’s a good point in human history to have worn-out hips, and things will probably get even better in the future.
Milestones Reached
A few thoughts on the key milestones that you have to reach to get cleared to go home from the hospital ..
They want to see your appetite return to normal, because you need lots of protein and general nutrition to heal. When I met with the surgeon’s PA four days before the surgery, he had told me “don’t be dieting or trying to lose weight after the surgery. Your body needs to heal, so if you feel like a cheeseburger, get the cheeseburger. If you want a chocolate shake with it, get the shake.” You don’t hear that type of advice from doctors very often.
I thought of him when I ordered my dinner the first day, and I went for the cheeseburger. I choked down two bites of it, and that was all I could stand. Things got steadily better on the appetite front with each meal, and for lunch on the final day I enthusiastically devoured a Reuben sandwich.

I was on oxygen after surgery, and they tried to remove it a few hours later (when I was light-headed and unable to attempt my first walk), but my oxygen saturation number dropped too far so they put me back on oxygen for a few more hours. I was fine without it after that.
They removed my drain about 20 hours after surgery, as mentioned above. They removed my saline drip IV on the second afternoon (so I became responsible for my own hydration), and they removed my catheter a couple hours later. As with many men during hospital stays, I can report that catheter removal was my least favorite moment of the whole ordeal, but there were no complications.
So for the second night in the hospital, I had no tubes or sensor anywhere on my body. It felt like a dry run for being at home, and I slept well, which was great.

Escape from Overlake
Dr. Bruckner visited me around 6:30 each morning to check on my status, and his visits were always preceded by a visit from his PA to check on my status and answer any questions about the process, schedule, etc. I like Dr. Bruckner’s style and that of every member of his team I’ve dealt with: they’re sharp, alert, consistently positive without being pollyannish, and extremely well-organized.
I should add that I’ve also heard several rave references from others who’ve had their hips replaced by Dr. Bruckner. In one amazing coincidence, the woman who delivered a gift basket from my co-workers told me that Dr. Bruckner had replaced her right hip five year ago and she’s thrilled with the results, no pain at all since the first few weeks. That’s a pretty reassuring reference to have randomly show up in my hospital room a few hours after surgery.
The morning of the third day, Dr. Bruckner said I was good to go home, we just needed to get sign-off from the physical therapist who would be running my group therapy session later in the morning. He asked me what the most important thing is going forward, and with a brief pause we both said in unison “don’t fall!”
A few hours later, I attended my final group therapy session and it all went well. I did the various exercises as well or better than anyone else in the room, which isn’t really anything to brag about: everyone else was either older, heavier or frailer than me (some all three), so it would have been a bad sign if I couldn’t stay ahead of them on the exercises.
A couple hours later, after a bunch of paperwork and getting a list of prescriptions filled, I was headed for home!
Summing Up: Not Yet
I’m only a week into this adventure, and I also have another hip to do in a few months, so it would be silly to sum things up at this point. I have much more to learn and experience, and I’ll write more as the process goes forward.
There are two key decision points coming up. About two weeks after surgery I’ll meet with Dr. Bruckner’s PA to check how things are healing and decide on any adjustments to my physical therapy plan, medications, and so on. And then six weeks after surgery I’ll meet with Dr. Bruckner himself for an assessment of how I’m recovering and to confirm the timing for the other hip surgery. If all goes as expected, I’ll get the left hip done during the holidays and by spring I’ll be back on the trails with Megan and the dogs.

When I left my hospital room, the photo hanging directly in front of me across the hall showed a woman and a white fluffy dog at Marymoor Dog Park, the dog park we most often visit with our dogs. I’m looking forward to returning to Marymoor with Megan and the dogs in the spring, and for many years to come.

UPDATE: After the second hip replacement 12 weeks later, I posted about that experience in Hip Replacement Isn’t What It Used To Be 12 Weeks Ago.